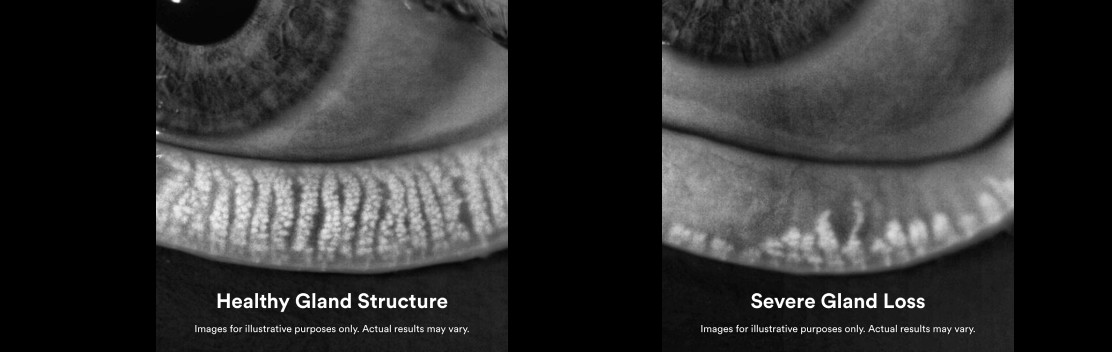
Meibomian Gland Dysfunction (MGD)
“Meibomian gland dysfunction (MGD) is a chronic, diffuse abnormality of the meibomian glands, commonly characterized by terminal duct obstruction and/or qualitative/quantitative changes in the glandular secretion. This may result in alteration of the tear film, symptoms of eye irritation, clinically apparent inflammation, and ocular surface disease.”
– TFOS MGD Report, 2011 (Official definition of the Meibomian Gland Dysfunction according to the Tear Film and Ocular Surface MGD Report)
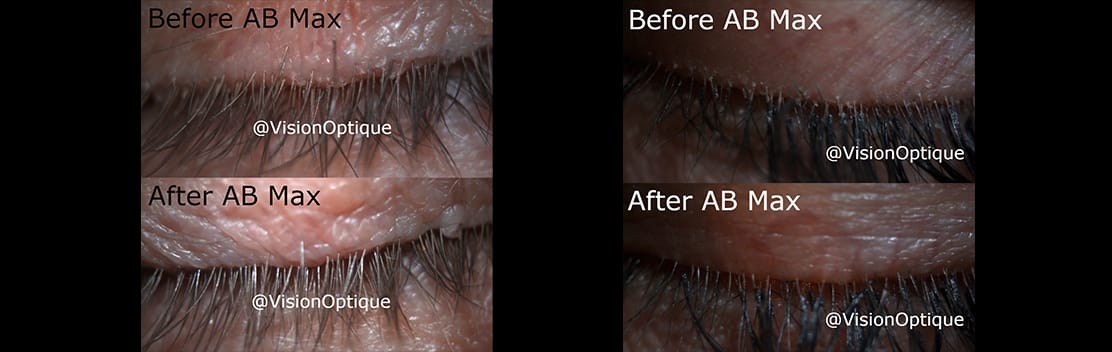
Meibomian gland dysfunction (MGD) is among the leading causes of dry eye disease and it affects millions of people around the world. Often reported symptoms are watery and burning eyes, fluctuating or blurry vision, and inability to wear contact lens or eye makeup. The most common type of MGD is obstructive MGD, which occurs when the glands become clogged, stopping the meibum from reaching the eye’s surface. The doctors at Vision Optique use the LipiFlow treatment, it is an FDA approved procedure to treat MGD.
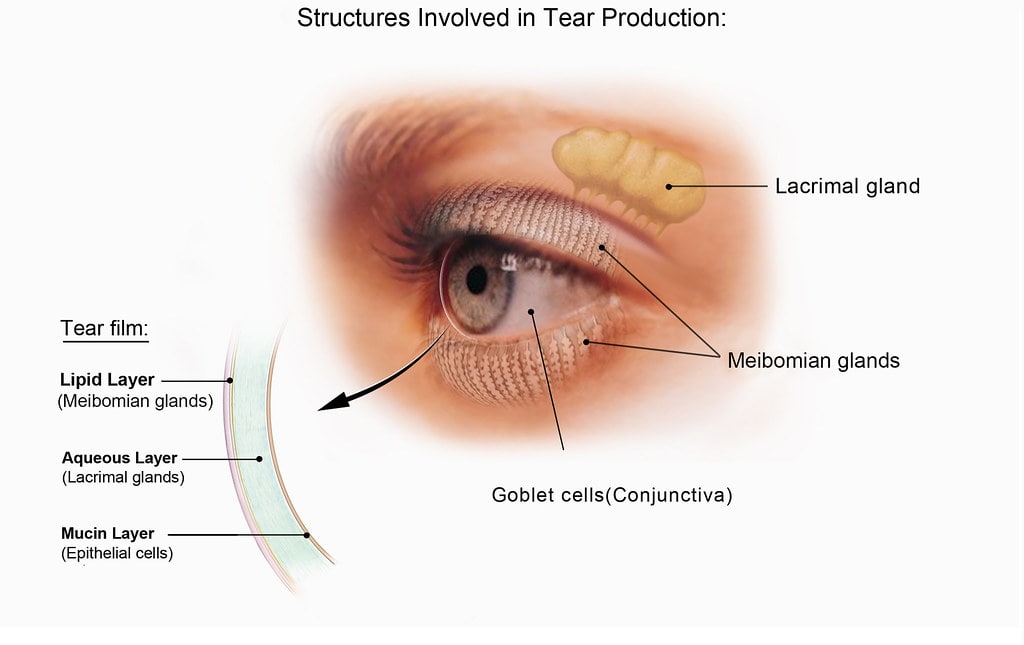
The meibomian glands secrete an oil called meibum. Meibum (oil), aqueous tear (watery layer), and mucin (mucus) make up the three layers of the tear film. The meibum/oil stabilizes the tear film and prevents it from evaporating too quickly. A healthy tear film is required to keep your eyes moist and comfortable.
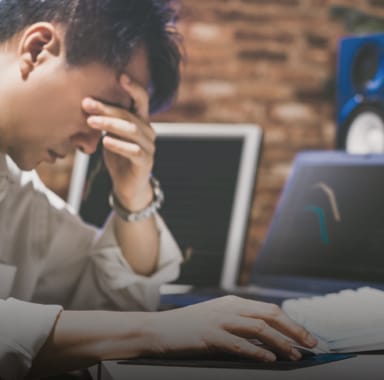
Spending long hours on digital devices (not blinking enough), wearing contact lenses, and using eyelash extensions or false eyelashes can all contribute to developing MGD.
Certain medical conditions can also cause MGD, such as:
- High cholesterol levels
- Conjunctivitis
- Eyelid infections
- Eyelid inflammation (blepharitis, Demodex)
- Skin disease (acne, rosacea, atopic and seborrhoeic dermatitis)
Additionally, some medications can cause a reduction in meibum production, such as glaucoma medications, estrogen replacement therapies, and retinoids commonly found in acne medication and anti-aging creams.
![]()